Suppose you are at work and your colleague next to you goes in an unconscious and not breathing mode. Are you going to wait for the doctor –even if he’s going to take one full hour – or are you going to apply your basic first aid knowledge to help him go through that medical crisis?
The best source of information and solution we have in cases of medical crises is a doctor. But, what do you do if there is no doctor around?
Panic is certainly not the answer.
Here’s what you should do in some circumstances.
How to Deal With Cuts and Scratches?

If you are unable to reach a doctor, follow these recommendations:
- Your hands must be washed thoroughly with clean water and soap.
- Get rid of any impurities by making the use of plain soap and boiled water cooled to room temperature.
- A sterile can be used or maybe a clean piece of cloth mixed in water and soap.
- A dry sterile dressing can also be used or one produced from a clean cloth.
- Make sure to inform the person to see a doctor as soon as possible if soreness develops.
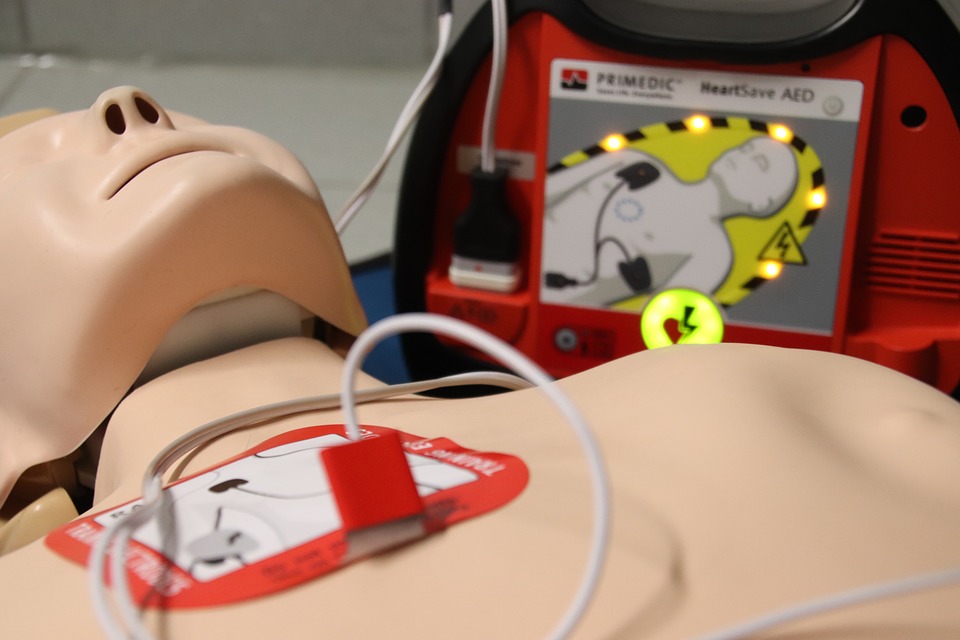
What to Do When Breathing Stops?

When breathing stops, immediate action is compulsory – this may mean the difference between life and death. A person may cease to breathe as a result of either disease or an accident. If breathing stops as a result of disease, artificial respiration efforts are of questionable value.
On the other hand, if breathing has stopped because of an accident, it is often possible to revive the person if there has not been too long an interval between the time the patient stopped breathing and the time the treatment is applied.
The causes of asphyxiation can be categorized into four groups:
- The supply of air is shut off completely, as in drowning, choking and strangling.
- There is an insufficient supply of oxygen in the air, as when a person is caught in an abandoned icebox, an empty silo, a vat and so on.
- The oxygen in the circulating blood has been displaced by other gases. This occurs in carbon-monoxide poisoning and also when a person is exposed to certain combinations of gases.
- In some cases, there is paralysis or depression of the breathing center, as from electric shock or drugs used to induce sleep.
Nonmedical people usually will not have the necessary training or experience to enable them to tell whether breathing has stopped because of a disease or an accident. It is best, therefore, to apply some form of artificial respiration in all cases until the cause of the condition can be determined by a competent physician.
An airway must be kept open from the lungs to the mouth if any form of artificial respiration is to be successful. It is important to clear the patient’s throat if it is blocked by foreign matter. The mouth must also be kept free from obstructions. If the person is discovered soon after his breathing has stopped and if artificial respiration is started immediately, his muscles usually retain enough tone so that it is not too hard to keep an airway open into the lungs. Alternately increasing and decreasing the size of the chest will force air in and out of the victim’s lungs if his throat and mouth are not obstructed. And, it might revive the person if body conditions permit life.
This increase and decrease can be accomplished either by blowing directly into the lungs through the mouth or nose or by alternately compressing and expanding the chest. The victim’s body position is relatively unimportant.
What to Do When a Poison Is Swallowed?

Poisonous substances like household cleaners, disinfectants and an overdose of medicine are accidentally taken by many people. In all cases, first, have the victim drink small amounts of plain water or milk in order to dilute the poison.
Sometimes the antidote for the poison can be printed on the label of the container of the poisonous material. It should be given to the victim if it is readily available.
In some cases, if there is a delay, it may be wise to induce vomiting, except when the victim is known to have taken an acid, an alkali or a petroleum product such as kerosene. In these cases, vomiting is strictly prohibited.
Now, in the second article, I’ll be talking about how to handle common emergencies like burns, cold injuries, heatstroke and so on. If you look forward to it, don’t forget to come back for part 2.